Health care system
Health care systems are designed to meet the health care needs of target populations. There are a wide variety of health care systems around the world. In some countries, health care system planning is distributed among market participants, whereas in others planning is made more centrally among governments, trade unions, charities, religious, or other co-ordinated bodies to deliver planned health care services targeted to the populations they serve. However, health care planning has often been evolutionary rather than revolutionary.[1]
Goals
The goals for health systems, according to the World Health Report 2000 - Health systems: improving performance (WHO, 2000), are good health, responsiveness to the expectations of the population, and fair financial contribution. Duckett (2004) proposed a two dimensional approach to evaluation of health care systems: quality, efficiency and acceptability on one dimension and equity on another.[2]
Providers
Health care providers are trained professional people working self-employed or as an employee in an organization, whether a for-profit company, a not-for profit company, a government entity, or a charity. Organizations employing people providing health care are also known as health care providers. Examples are doctors and nurses, paramedics, dentists, medical laboratory staff, specialist therapists, psychologists, pharmacists, chiropractors, and optometrists.
Financing
Aug2005.jpg)
There are generally five primary methods of funding health care systems:[3][4]
- direct or out-of-pocket payments,
- general taxation to the state, county or municipality,
- social health insurance,
- voluntary or private health insurance, and
- donations or community health insurance.
Most countries' systems feature a mix of all five models. One study [5] based on data from the OECD concluded that all types of health care finance "are compatible with" an efficient health care system. The study also found no relationship between financing and cost control.
The term health insurance is generally used to describe a form of insurance that pays for medical expenses. It is sometimes used more broadly to include insurance covering disability or long-term nursing or custodial care needs. It may be provided through a government-sponsored social insurance program, or from private insurance companies. It may be purchased on a group basis (e.g., by a firm to cover its employees) or purchased by individual consumers. In each case, the covered groups or individuals pay premiums or taxes to help protect themselves from high or unexpected health care expenses. Similar benefits paying for medical expenses may also be provided through schemes organized by the government and funded through contributions from users.
By estimating the overall cost of health care expenses, a routine finance structure (such as a monthly premium or annual tax) can be developed, ensuring that money is available to pay for the health care benefits specified in the insurance agreement. The benefit is administered by a central organization, most often either a government agency or a private or not-for-profit entity operating a health plan.[6]
Many forms of commercial health insurance control their costs by restricting the benefits that are paid by through deductibles, co-payments, coinsurance, policy exclusions, and total coverage limits and will severely restrict or refuse coverage of pre-existing conditions. Many government schemes also have co-payment schemes but exclusions are rare because of political pressure. The larger insurance schemes may also negotiate fees with providers.
Many forms of government insurance schemes control their costs by using the bargaining power of government to control costs in the health care delivery system. For example by negotiating drug prices directly with pharmaceutical companies, or negotiating standard fees with the medical profession. Government schemes sometimes feature contributions related to earnings as part of a scheme to deliver universal health care, which may or may not also involve the use of commercial and non-commercial insurers. Essentially the more wealthy pay proportionately more into the scheme to cover the needs of the relatively poor who therefore contribute proportionately less. There are usually caps on the contributions of the wealthy and minimum payments that must be made by the insured (often in the form of a minimum contribution, similar to a deductible in commercial insurance models). In health care delivery system (primary health care) there are also providers in different ways, for example Government, private, NGOs and traditional medicine.
Payment models
Primary care
There are three ways to pay general practitioners. There has been growing interest in blending elements of these systems.[7]
Fee-for-service
Fee-for-service arrangements pay general practitioners based on the service.[7] They are even more widely used for specialists working in ambulatory care.[7]
There are two ways to set fee levels:[7]
- By individual practitioners.
- Central negotiations (as in Japan, Germany, Canada and in France) or hybrid model (such as in Australia, France's sector 2, and New Zealand) where GPs can charge extra fees on top of standardized patient reimbursement rates.
Other
In capitation payment systems, GPs are paid for each patient on their "list", usually with adjustments for factors such as age and gender.[7] According to OECD, "these systems are used in Italy (with some fees), in all four countries of the United Kingdom (with some fees and allowances for specific services), Austria (with fees for specific services), Denmark (one third of income with remainder fee for service), Ireland (since 1989), the Netherlands (fee-for-service for privately insured patients and public employees) and Sweden (from 1994). Capitation payments have become more frequent in “managed care” environments in the United States."[7]
According to OECD, "Capitation systems allow funders to control the overall level of primary health expenditures, and the allocation of funding among GPs is determined by patient registrations. However, under this approach, GPs may register too many patients and under-serve them, select the better risks and refer on patients who could have been treated by the GP directly. Freedom of consumer choice over doctors, coupled with the principle of "money following the patient" may moderate some of these risks. Aside from selection, these problems are likely to be less marked than under salary-type arrangements."[7]
In several OECD countries, general practitioners (GPs) are employed on salaries for the government.[7] According to OECD, "Salary arrangements allow funders to control primary care costs directly; however, they may lead to under-provision of services (to ease workloads), excessive referrals to secondary providers and lack of attention to the preferences of patients."[7] There has been movement away from this system.[7]
Health informatics
Health informatics or medical informatics is the intersection of information science, medicine and health care. It deals with the resources, devices and methods required to optimize the acquisition, storage, retrieval and use of information in health and biomedicine. Health informatics tools include not only computers but also clinical guidelines, formal medical terminologies, and information and communication systems.
Management
Public health is concerned with threats to the overall health of a community based on population health analysis. The population in question can be as small as a handful of people or as large as all the inhabitants of several continents (for instance, in the case of a pandemic). Public health is typically divided into epidemiology, biostatistics and health services. Environmental, social, behavioral, and occupational health are also important subfields.

Vaccination policy refers to the policy a government adopts in relation to vaccination. Vaccinations are voluntary in some countries and mandatory in some countries. Some governments pay all or part of the costs of vaccinations for vaccines in a national vaccination schedule.
Today, most governments recognize the importance of public health programs in reducing the incidence of disease, disability, and the effects of aging, although public health generally receives significantly less government funding compared with medicine. In recent years, public health programs providing vaccinations have made incredible strides in promoting health, including the eradication of smallpox, a disease that plagued humanity for thousands of years.
An important public health issue facing the world currently is HIV/AIDS[8]. Another major public health concern is diabetes[9]. In 2006, according to the World Health Organization, at least 171 million people worldwide suffered from diabetes. Its incidence is increasing rapidly, and it is estimated that by the year 2030, this number will double. A controversial aspect of public health is the control of smoking[10].
Antibiotic resistance is another major concern, leading to the reemergence of diseases such as Tuberculosis.
Special health care systems
- Occupational safety and health
- School health services
- Military medicine
Cross-country comparisons
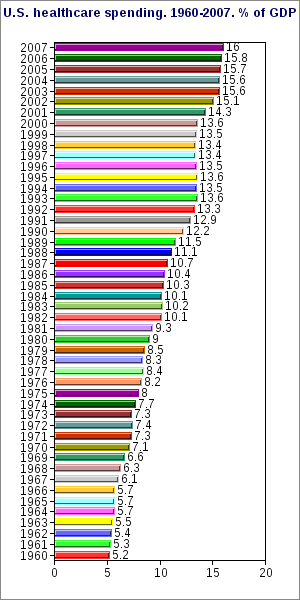
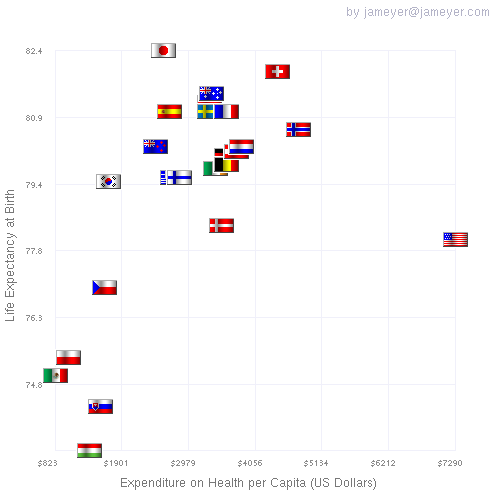
Direct comparisons of health statistics across nations are complex. The Commonwealth Fund, in its annual survey, "Mirror, Mirror on the Wall", compares the performance of the health care systems in Australia, New Zealand, the United Kingdom, Germany, Canada and the U.S. Its 2007 study found that, although the U.S. system is the most expensive, it consistently underperforms compared to the other countries.[11] A major difference between the U.S. and the other countries in the study is that the U.S. is the only country without universal health care. The OECD also collects comparative statistics, and has published brief country profiles.[12][13][14]
| Country | Life expectancy | Infant mortality rate | Physicians per 1000 people | Nurses per 1000 people | Per capita expenditure on health (USD) | Healthcare costs as a percent of GDP | % of government revenue spent on health | % of health costs paid by government |
|---|---|---|---|---|---|---|---|---|
| Australia | 81.4 | 4.2 | 2.8 | 9.7 | 3,137 | 8.7 | 17.7 | 67.7 |
| Canada | 80.7 | 5.0 | 2.2 | 9.0 | 3,895 | 10.1 | 16.7 | 69.8 |
| France | 81.0 | 4.0 | 3.4 | 7.7 | 3,601 | 11.0 | 14.2 | 79.0 |
| Germany | 79.8 | 3.8 | 3.5 | 9.9 | 3,588 | 10.4 | 17.6 | 76.9 |
| Japan | 82.6 | 2.6 | 2.1 | 9.4 | 2,581 | 8.1 | 16.8 | 81.3 |
| Norway | 80.0 | 3.0 | 3.8 | 16.2 | 5,910 | 9.0 | 17.9 | 83.6 |
| Sweden | 81.0 | 2.5 | 3.6 | 10.8 | 3,323 | 9.2 | 13.6 | 81.7 |
| UK | 79.1 | 4.8 | 2.5 | 10.0 | 2,992 | 8.4 | 15.8 | 81.7 |
| USA | 78.1 | 6.7 | 2.4 | 10.6 | 7,290 | 16.0 | 18.5 | 45.4 |
Life Expectancy vs Health Care Spending in 2007 for OECD Countries. The data source is http://www.oecd.org and the image was built at http://flagscatter.com
Health care by country
Afghanistan
Beginning in 1979, military conflict destroyed the health system of Afghanistan. Most medical professionals left the country in the 1980s and 1990s, and all medical training programmes ceased.[15] In 2004 Afghanistan had one medical facility for every 27,000 people, and some centers were responsible for as many as 300,000 people.[15] In 2004 international organizations provided a large share of medical care.[15] An estimated one-quarter of the population had no access to health care.[15] In 2003 there were 11 physicians and 18 nurses per 100,000 population, and the per capita health expenditure was US$28.[15]
Algeria
Health in Algeria, according to information from a March 6, 2006 United States report, does not compare well with the developed world. Algeria has inadequate numbers of physicians (one per 1,000 people) and hospital beds (2.1 per 1,000 people) and poor access to water (87 percent of the population) and sanitation (92 percent of the population). Given Algeria’s young population, policy favors preventive health care and clinics over hospitals. In keeping with this policy, the government maintains an immunization program. However, poor sanitation and unclean water still cause tuberculosis, hepatitis, measles, typhoid fever, cholera, and dysentery. In 2003 about 0.10 percent of the population aged 15–49 was living with human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS). The poor generally receive health care free of charge, but the wealthy pay for care according to a sliding scale. Access to health care is enhanced by the requirement that doctors and dentists work in public health for at least five years. However, doctors are more easily found in the cities of the north than in the southern Sahara region.
Argentina
Argentina’s health care system is composed of three sectors: the public sector, financed through taxes; the private sector, financed through voluntary insurance schemes; and the social security sector, financed through obligatory insurance schemes. The Ministry of Health and Social Action (MSAS), oversees all three subsectors of the health care system and is responsible for setting of regulation, evaluation and collecting statistics.
Argentina has three sectors. The public sector is funded and managed by Obras Sociales, umbrella organizations for Argentine worker's unions. There are over 300 Obras Sociales in Argentina, each chapter being organized according to the occupation of the beneficiary. These organizations vary greatly in quality and effectiveness. The top 30 chapters hold 73% of the beneficiaries and 75% of resources for all Obras Sociales schemes and the monthly average a beneficiary receives varies from $5–80 per month.[16] MSAS has established a Solidarity Redistribution Fund (FSR) to try to address these beneficiary inequities. Only workers employed in the formal sector are covered under Obras Sociales insurance schemes and after Argentina’s economic crisis of 2001, the number of those covered under these schemes fell slightly (as unemployment increased and employment in the informal sector rose). In 1999, there were 8.9 million beneficiaries covered by Obras Sociales.[17] The private health care sector in Argentina is characterized by great heterogeneity and is made up of a great number of fragmented facilities and small networks; it consists of over 200 organizations and covers approximately 2 million Argentines.[16] Private insurance often overlaps with other forms of health care coverage, thus it is difficult to estimate the degree to which beneficiaries are dependent on the public and private sectors. According to a 2000 report by the IRBC, foreign competition has increased in Argentina’s private sector, with Swiss, American and other Latin American health care providers entering the market in recent years. This has been accompanied by little formal regulation.[16] The public system serves those not covered by Obras Sociales or private insurance schemes. It also provides emergency services. According to above-mentioned IRBC report, Argentina’s public system exhibits serious structural deterioration and managerial inefficiency; a high degree of administrative centralization at the provincial level; rigidity in its staffing structure and labour relationships; no adequate system of incentives; inadequate information systems on which to base decision-making and control; serious deficits in facilities and equipment maintenance; and a system of management ill-suited to its size. The public system is highly decentralized to the provincial level; often primary care is even under the purview of local townships. Since 2001, the number of Argentines relying on public services has seen an increase. According to 2000 figures, 37.4% of Argentines had no health insurance, 48.8 were covered under Obras Sociales, 8.6% had private insurance, and 3.8% were covered by both Obras Sociales and private insurance schemes.[17] But even with this inefficiency, everyone can get medical attention for free (even surgery) with doctors that will do whatever they can to heal the patient.
Australia
In Australia the current system, known as Medicare, was instituted in 1984. It coexists with a private health system. All legal permanent residents are entitled to free public hospital care. Treatment by private doctors is also free when the doctor direct bills the Health Department (Bulk Billing). Medicare is funded partly by a 1.5% income tax levy (with exceptions for low-income earners), but mostly out of general revenue. An additional levy of 1% is imposed on high-income earners without private health insurance. There is an uncapped 30% subsidy on private health insurance. As well as Medicare, there is a separate Pharmaceutical Benefits Scheme under which listing and a government subsidy is dependent on expert evaluation of the comparative cost-effectiveness of new pharmaceuticals. In 2005, Australia spent 8.8% of GDP on health care, or US$3,181 per capita. Of that, approximately 67% was government expenditure.[18]
Belgium
As in most countries, the system divides itself into state and private, though fees are payable in both. A person needs to have adequate coverage through either the state insurance or through private insurance. In the state mutuelle/mutualiteit scheme a person has the ability to choose any doctor, clinic or hospital you like, in any location and without referral, according to your needs in much the same way as you can with private insurance.
- Doctors
General practitioners can be found in private practices or attached to clinics and hospitals. A person is free to consult or register with any of their own choosing. Similarly with specialist consultants. Consultations usually end with a handing over of money and very few doctors offer payment by card of any type. Reimbursements are available for those with insurance, either private or public. If a patient is on a private scheme, or is uninsured, the fee is payable in full at the time of the appointment.
The majority of dentists in Belgium are private, though there are those who accept part-payment on state insurance.
As with general practitioners, people in Belgium can arrange to see a specialist of choice at any hospital. Those going into hospital for a planned stay need to take personal care items such as a towel and soap with them as these are not generally provided.
In Brussels the eleven big public hospitals are organized under the Iris association. [3])
- Alternative health care
The Ministry of Health recognizes homeopathy, acupuncture, osteopathy and chiropractic as reimbursable alternative treatments. Reimbursement is possible only if the practitioner is registered as a qualified doctor.
- Emergency treatment
If a call is made to the Emergency services using the old emergency 100 or the common European 112 telephone number, an ambulance will take transport the patient to the nearest emergency centre or the best centre suited according to need, for example, a specialist burns unit.
- Pharmacies
Pharmacies are ubiquitous in Belgium, with the green cross sign everywhere. There is a rota system for chemists to open outside of usual hours and through the night.
- Insurance
Health care insurance is a part of the Belgian social security system. To benefit a person must join a health insurance fund mutuelle (mutualité) or ziekenfonds (mutualiteit) for which an employer's certificate is required if the employer is to contribute to the cost. If employed a person's contributions is automatically deducted from salary. The employer will also pay a contribution. Health insurance funds will reimburse medical costs. The choice of mutual insurer is up to the individual. Most of them are affiliated to a religious or political institution but there is no real difference between them because reimbursement rates are fixed by the Belgian government.
Insurance funds do not cover 100 per cent of your bills and typical reimbursement is between half to three-quarters of a typical doctors or specialists visit.
Insured persons have a standardized credit card style SIS-card[19] which is needed in pharmacies and hospitals.
Bhutan
Bhutan's health care system development accelerated in the early 1960s with the establishment of the Department of Public Health and the opening of new hospitals and dispensaries throughout the country. By the early 1990s, health care was provided through twenty-nine general hospitals (including five leprosy hospitals, three army hospitals, and one mobile hospital), forty-six dispensaries, sixty-seven basic health units, four indigenous-medicine dispensaries, and fifteen malaria eradication centers. The major hospitals were the National Referral Hospital in Thimphu, and other hospitals in Geylegphug, and Tashigang. Hospital beds in 1988 totaled 932. There was a severe shortage of health-care personnel with official statistics reporting only 142 physicians and 678 paramedics, about one health-care professional for every 2,000 people, or only one physician for almost 10,000 people. Training for health-care assistants, nurses' aides, midwives, and primary health-care workers was provided at the Royal Institute of Health Sciences, associated with Thimphu General Hospital, which was established in 1974. Graduates of the school were the core of the national public health system and helped staff the primary care basic health units throughout the country. Additional health-care workers were recruited from among volunteers in villages to supplement primary health care.[20] The Institute of Traditional Medicine Services supports indigenous medical centers associated with the district hospitals.
Brazil
The Brazilian health system is composed of a large public, government managed system, the SUS (Sistema Único de Saúde) , which serves the majority of the population, and a private sector, managed by health insurance funds and private entrepreneurs.
The public health system, SUS, was established in 1988 by the Brazilian Constitution, and sits on 3 basic principles of universality, comprehensiveness and equity. Universality states that all citizens must have access to health care services, without any form of discrimination, regarding skin color, income, social status, gender or any other variable.
Government standards state that citizen's health is the result of multiple variables, including employment, income, access to land, sanitation services, access and quality of health services, education, psychic, social and family conditions, and are entitled to full and complete health care, comprising prevention, treatment and rehabilitation. Equity states that health policies should be oriented towards the reduction of inequalities between population groups and individuals, being the most needed the ones for whom policies should be first directed.
SUS has also guidelines for its implementation, the most peculiar being popular participation, which defines that all policies are to be planned and supervised directly by the population, through local, city, state and national health councils en conferences. This is regarded as a very advanced form of direct democracy and has established the guidelines for many similar initiatives in sectors other than health all over Brazilian society.
The level of public spending is particularly high in relation to GDP for a country of Brazil’s income level and in comparison with its emerging-market peers. Government outlays on health care alone account for nearly 9% of GDP, the second largest item of spending following social protection. In health care, a number of conventional output indicators are not out of step with OECD averages. Following the decentralisation of service delivery in the early 1990s, increasing emphasis has appropriately been placed on enhancing preventive care. But, in a decentralised setting, cost-effectiveness depends a great deal on the ability of service deliverers to exploit economies of scale and scope. Experience with inter-municipal initiatives for procurement, as well as flexible arrangements for hospital administration and human-resource management, is by and large positive.
Private Health Insurance is widely available in Brazil and may be purchased on an individual-basis or obtained as a work benefit (major employers usually offer private health insurance benefits). Public health care is still accessible for those who choose to obtain private health insurance. As of March, 2007, more than 37 million Brazilians had some sort of private health insurance.[21]
Bulgaria
Bulgaria began overall reform of its antiquated health system, inherited from the communist era, only in 1999. In the 1990s, private medical practices expanded somewhat, but most Bulgarians relied on communist-era public clinics while paying high prices for special care. During that period, national health indicators generally worsened as economic crises substantially decreased health funding. The subsequent health reform program has introduced mandatory employee health insurance through the National Health Insurance Fund (NHIF), which since 2000 has paid a gradually increasing portion of primary health-care costs. Employees and employers pay an increasing, mandatory percentage of salaries, with the goal of gradually reducing state support of health care. Private health insurance plays only a supplementary role. The system also has been decentralized by making municipalities responsible for their own health-care facilities, and by 2005 most primary care came from private physicians. Pharmaceutical distribution also was decentralized.[15]
In the early 2000s, the hospital system was reduced substantially to limit reliance on hospitals for routine care. Anticipated membership in the European Union (2007) was a major motivation for this trend. Between 2002 and 2003, the number of hospital beds was reduced by 56 percent to 24,300. However, the pace of reduction slowed in the early 2000s; in 2004 some 258 hospitals were in operation, compared with the estimated optimal number of 140. Between 2002 and 2004, health-care expenditures in the national budget increased from 3.8 percent to 4.3 percent, with the NHIF accounting for more than 60 percent of annual expenditures.[15]
In the 1990s, the quality of medical research and training decreased seriously because of low funding. In the early 2000s, the emphasis of medical and paramedical training, which was conducted in five medical schools, was preparation of primary-care personnel to overcome shortages resulting from the communist system’s long-term emphasis on training specialists. Experts considered that Bulgaria had an adequate supply of doctors but a shortage of other medical personnel. In 2000 Bulgaria had 3.4 doctors, 3.9 nurses, and 0.5 midwives per 1,000 population.[15]
Canada
Canada has a federally sponsored, publicly funded Medicare system, with most services provided by the private sector. Each province may opt out, though none currently does. Some provinces still charge premiums to individuals and families. Many employers also offer additional health coverage as a benefit. Canada's system is known as a single payer system, where basic services are provided by private doctors, (since 2002 they have been allowed to incorporate), with the entire fee paid for by the government at the same rate. Most family doctors receive a fee per visit. These rates are negotiated between the provincial governments and the province's medical associations, usually on an annual basis. A physician cannot charge a fee for a service that is higher than the negotiated rate — even to patients who are not covered by the publicly funded system — unless he or she opts out of billing the publicly funded system altogether. Pharmaceutical costs are set at a global median by government price controls. Other areas of health care, such as dentistry and optometry, are wholly private although in some provinces, emergency cases visit to optometrists are partly covered by medicare. In 2005, Canada spent 9.8% of GDP on health care, or US$3,463 per capita. Of that, approximately 70% was government expenditure.[18]
Cape Verde
Medical facilities in Cape Verde are limited, and some medicines are in short supply or unavailable. There are hospitals in Praia and Mindelo, with smaller medical facilities in other places. The islands of Brava and Santo Antão no longer have functioning airports so air evacuation in the event of a medical emergency is nearly impossible from these two islands. Brava also has limited inter-island ferry service.[22]
Chile
Chile has maintained a dual health care system in which its citizens can voluntarily opt for coverage by either the public National Health Insurance Fund or any of the country's private health insurance companies. 68% of the population is covered by the public fund and 18% by private companies. The remaining 14% is covered by other not-for-profit agencies or has no specific coverage. The system's duality has led to increasing inequalities prompting the Chilean government to introduce major reforms in health care provision. Chile's health care system is funded by a universal income tax deduction equal to 7% of every worker's wage. Many private health insurance companies encourage people to pay a variable extra on top of the 7% premium to upgrade their basic health plans. Because of this arrangement, the public and private health subsystems have existed almost completely separate from each other rather than coordinating to achieve common health objectives.[23]
Costa Rica
Costa Rica provides universal health care to its citizens and permanent residents.
Cuba
Health care in Cuba consists of a government-coordinated system that guarantees universal coverage and consumes a lower proportion of the nation's GDP (7.3%) than some highly privatised systems (e.g. USA: 16%) (OECD 2008). The system does charge fees in treating elective treatment for patients from abroad, but tourists who fall ill are treated free in Cuban hospitals. Cuba attracts patients mostly from Latin America and Europe by offering care of comparable quality to a developed nation but at much lower prices. Cuba's own health indicators are the best in Latin America and surpass those of the US in some respects (infant mortality rates, underweight babies, HIV infection, immunisation rates, doctor per population rates). (UNDP 2006: Tables 6,7,9,10) In 2005, Cuba spent 7.6% of GDP on health care, or US$310 per capita. Of that, approximately 91% was government expenditure.[18]
Denmark
Denmark's health care system has retained the same basic structure since the early 1970s. The administration of hospitals and personnel is dealt with by the Ministry of the Interior, while primary care facilities, health insurance, and community care are the responsibility of the Ministry of Social Affairs. Anyone can go to a physician for no fee and the public health system entitles each Dane to his/her own doctor. Expert medical/surgical aid is available, with a qualified nursing staff. Costs are borne by public authorities, but high taxes contribute to these costs. As of 1999, there were an estimated 3.4 physicians and 4.5 hospital beds per 1,000 people. The number of hospital beds, like that in other EU countries, has undergone a major decline since 1980, from around 40,000 to about 23,000 in 1998/99. Deinstitutionalization of psychiatric patients has contributed significantly to this trend. The ratio of doctors to population, by contrast, has increased during this period.
The total fertility rate in 2000 was 1.7, while the maternal mortality rate was 10 per 100,000 live births as of 1998. Studies show that between 1980 and 1993, 63% of married women (ages 15 to 49) used contraception. As of 2002 cardiovascular diseases and cancer were the leading causes of death. Denmark's cancer rates were the highest in the European Union. In 1999, there were only 12 reported cases of tuberculosis per 100,000 people. As of 1999, the number of people living with HIV/AIDS was estimated at 4,300 and deaths from AIDS that year were estimated at less than 100. HIV prevalence was 0.17 per 100 adults.
Danish citizens may choose between two systems of primary health care: medical care provided free of charge by a doctor whom the individual chooses for a year and by those specialists to whom the doctor refers the patient; or complete freedom of choice of any physician or specialist at any time, with state reimbursement of about two-thirds of the cost for medical bills paid directly by the patient. Most Danes opt for the former. All patients receive subsidies on pharmaceuticals and vital drugs; everyone must pay a share of dental bills. As of 1999, total health care expenditure was estimated at 8.4% of GDP.
Responsibility for the public hospital service rests with county authorities. Counties form public hospital regions, each of which is allotted one or two larger hospitals with specialists and two to four smaller hospitals where medical treatment is practically free. State-appointed medical health officers, responsible to the National Board of Health, are employed to advise local governments on health matters. Public health authorities have waged large-scale campaigns against tuberculosis, venereal diseases, diphtheria, and poliomyelitis. The free guidance and assistance given to mothers of newborn children by public health nurses have resulted in a low infant mortality rate of 4 per 1,000 live births (2000). Medical treatment is free up to school age, when free school medical inspections begin. As of 1999, children up to one year of age were vaccinated against diphtheria, pertussis, and tetanus (99%) and measles (92%). In 2000, life expectancy at birth was 76 years for males and females. The overall death rate was 11 per 1,000 people in 1999.
Read more: Health - Denmark - system http://www.nationsencyclopedia.com/Europe/Denmark-HEALTH.html#ixzz0kk32t7BP
Eritrea
Health in Eritrea is generally poor as it remains one of the poorest countries in the world. About one-third of the population lives in extreme poverty, and more than half survives on less than US$1 per day. Health care and welfare resources generally are believed to be poor, although reliable information about conditions is often difficult to obtain. In 2001, the most recent year for which figures are available, the Eritrean government spent 5.7 percent of gross domestic product on national health accounts. The World Health Organization (WHO) estimated that in 2004 there were only three physicians per 100,000 people in Eritrea. The two-year war with Ethiopia, coming on the heels of a 30-year struggle for independence, negatively affected the health sector and the general welfare. The rate of prevalence of human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS), although low by sub-Saharan African standards, was high enough at 2.7 percent in 2003 to be considered a generalized epidemic. In the decade since 1995, however, impressive results have been achieved in lowering maternal and child mortality rates and in immunizing children against childhood diseases. In 2003 average life expectancy was slightly less than 53 years, according to the WHO.
Ethiopia
Throughout the 1990s, the government, as part of its reconstruction program, devoted ever-increasing amounts of funding to the social and health sectors, which brought corresponding improvements in school enrollments, adult literacy, and infant mortality rates. These expenditures stagnated or declined during the 1998–2000 war with Eritrea, but in the years since, outlays for health have grown steadily. In 2000–2001, the budget allocation for the health sector was approximately US$144 million; health expenditures per capita were estimated at US$4.50, compared with US$10 on average in sub-Saharan Africa. In 2000 the country counted one hospital bed per 4,900 population and more than 27,000 people per primary health care facility. The physician to population ratio was 1:48,000, the nurse to population ratio, 1:12,000. Overall, there were 20 trained health providers per 100,000 inhabitants. These ratios have since shown some improvement. Health care is disproportionately available in urban centers; in rural areas where the vast majority of the population resides, access to health care varies from limited to nonexistent. As of the end of 2003, the United Nations (UN) reported that 4.4 percent of adults were infected with human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS); other estimates of the rate of infection ranged from a low of 7 percent to a high of 18 percent. Whatever the actual rate, the prevalence of HIV/AIDS has contributed to falling life expectancy since the early 1990s. According to the Ministry of Health, one-third of current young adult deaths are AIDS-related. Malnutrition is widespread, especially among children, as is food insecurity. Because of growing population pressure on agricultural and pastoral land, soil degradation, and severe droughts that have occurred each decade since the 1970s, per capita food production is declining. According to the UN and the World Bank, Ethiopia at present suffers from a structural food deficit such that even in the most productive years, at least 5 million Ethiopians require food relief.[15]
In 2002 the government embarked on a poverty reduction program that called for outlays in education, health, sanitation, and water. A polio vaccination campaign for 14 million children has been carried out, and a program to resettle some 2 million subsistence farmers is underway. In November 2004, the government launched a five-year program to expand primary health care. In January 2005, it began distributing antiretroviral drugs, hoping to reach up to 30,000 HIV-infected adults.[15]
Finland
In Finland, public medical services at clinics and hospitals are run by the municipalities (local government) and are funded 78% by taxation, 20% by patients through access charges, and by others 2%. Patient access charges are subject to annual caps. For example GP visits are (11€ per visit with annual 33€ cap), hospital outpatient treatment (22€ per visit), a hospital stay, including food, medical care and medicines (26€ per 24 hours, or 12€ if in a psychiatric hospital). After a patient has spent 590€ per year on public medical services, all treatment and medications thereafter are free. Taxation funding is partly local and partly nationally based. Patients can claim re-imbursement of part of their prescription costs from KELA. Finland also has a much smaller private medical sector which accounts for about 14 percent of total health care spending. Only 8% of doctors choose to work in private practice, and some of these also choose to do some work in the public sector. Private sector patients can claim a contribution from KELA towards their private medical costs (including dentistry) if they choose to be treated in the more expensive private sector, or they can join private insurance funds. However, private sector health care is mainly in the primary care sector. There are virtually no private hospitals, the main hospitals being either municipally owned (funded from local taxes) or run by the teaching universities (funded jointly by the municipalities and the national government). In 2005, Finland spent 7.5% of GDP on health care, or US$2,824 per capita. Of that, approximately 78% was government expenditure.[18]
France
In France, most doctors remain in private practice; there are both private and public hospitals. Social Security consists of several public organizations, distinct from the state government, with separate budgets that refunds patients for care in both private and public facilities. It generally refunds patients 70% of most health care costs, and 100% in case of costly or long-term ailments. Supplemental coverage may be bought from private insurers, most of them nonprofit, mutual insurers, to the point that the word "mutuelle" (mutual) has come to be a synonym of supplemental private insurer in common language. Until recently, social security coverage was restricted to those who contributed to social security (generally, workers or retirees), excluding some poor segments of the population; the government of Lionel Jospin put into place the "universal health coverage". In some systems, patients can also take private health insurance, but choose to receive care at public hospitals, if allowed by the private insurer.
In its 2000 assessment of world health care systems, the World Health Organization found that France provided the "best overall health care" in the world.[24] In 2005, France spent 11.2% of GDP on health care, or US$3,926 per capita. Of that, approximately 80% was government expenditure.[18]
Germany
Germany has a universal multi-payer system with two main types of health insurance: "State health insurance" (Gesetzliche Krankenversicherung) known as sickness funds and "Private" (Private Krankenversicherung).[25][26][27] Compulsory insurance applies to those below a set income level and is provided through private non-profit "sickness funds" at common rates for all members, and is paid for with joint employer-employee contributions. Provider compensation rates are negotiated in complex corporatist social bargaining among specified autonomously organized interest groups (e.g. physicians' associations) at the level of federal states (Länder). The sickness funds are mandated to provide a wide range of coverages and cannot refuse membership or otherwise discriminate on an actuarial basis. Small numbers of persons are covered by tax-funded government employee insurance or social welfare insurance. Persons with incomes above the prescribed compulsory insurance level may opt into the sickness fund system, which a majority do, or purchase private insurance. Private supplementary insurance to the sickness funds of various sorts is available. In 2005, Germany spent 10.7% of GDP on health care, or US$3,628 per capita. Of that, approximately 77% was government expenditure.[18]
Ghana
In Ghana, most health care is provided by the government, but hospitals and clinics run by religious groups also play an important role. Some for-profit clinics exist, but they provide less than 2% of health services. Health care is very variable through the country. The major urban centres are well served, but rural areas often have no modern health care. Patients in these areas either rely on traditional medicine or travel great distances for care. In 2005, Ghana spent 6.2% of GDP on health care, or US$30 per capita. Of that, approximately 34% was government expenditure.[18]
India
In the greater India, the hospitals are run by government, charitable trusts and by private organizations. The government hospitals in rural areas are called the (PHC)s primary health centre. Major hospitals are located in district head quarters or major cities. Apart from the modern system of medicine, traditional and indigenous medicinal systems like Ayurvedic and Unani systems are in practice throughout the country. The Modern System of Medicine is regulated by the Medical Council of India, whereas the Alternative systems recognised by Government of India are regulated by the Department of AYUSH (an acronym for Ayurveda, Yunani, Siddha & Homeopathy) under the Ministry of Health, Government of India. PHCs are non-existent in most places, due to poor pay and scarcity of resources. Patients generally prefer private health clinics. These days some of the major corporate hospitals are attracting patients from neighboring countries such as Pakistan, countries in the Middle East and some European countries by providing quality treatment at low cost. In 2005, India spent 5% of GDP on health care, or US$36 per capita. Of that, approximately 19% was government expenditure.[18], but now the situation is changing.
Indonesia
Indonesia had a three-tiered system of community health centers in the late 1990s, with 0.66 hospital beds per 1,000 population, the lowest rate among members of the Association of Southeast Asian Nations (ASEAN).[15] In the mid-1990s, according to the World Health Organization (WHO), there were 16 physicians per 100,000 population in Indonesia, 50 nurses per 100,000, and 26 midwives per 100,000.[15] Both traditional and modern health practices are employed. Government health expenditures are about 3.7 percent of the gross domestic product (GDP).[15] There is about a 75:25 percent ratio of public to private health-care expenditures.
Ireland
For Northern Ireland, see Health and Social Care in Northern Ireland. In 2005, Ireland spent 8.2% of GDP on health care, or US$3,996 per capita. Of that, approximately 79% was government expenditure.[18]
Israel
In Israel, the publicly funded medical system is universal and compulsory. In 2005, Israel spent 7.8% of GDP on health care, or US$1,533 per capita. Of that, approximately 66% was government expenditure.[18]
Italy
According to WHO in 2000, Italy had the world's "second overall best" healthcare system in the world, coming after France, and surpassing Spain, Oman and Japan.[28]
In 1978 Italy adopted a tax-funded universal health care system called "National Health Service" (in Italian: Servizio Sanitario Nazionale), which was closely modeled on the British system. The SSN covers general practice (distinct between adult and pediatric practice), outpatient and inpatient treatments, and the cost of most (but not all) drugs and sanitary ware.[29] The government sets LEA (fundamental levels of care, Livelli essenziali di assistenza in Italian) which cover all necessary treatments, which the state must guarantee to all for free or for a "ticket", a share of the costs (but various categories are exempted).[30] The public system has also the duty of prevention at place of work and in the general environment. A private sector also exists, with a minority role in medicine but a principal role in dental health, as most people prefer private dental services.
In Italy the public system has the unique feature of paying general practitioners a fee per capita per year, a salary system, that does not reward repeat visits, testing, and referrals.[31] While there is a paucity of nurses, Italy has one of the highest doctor per capita ratios at 3.9 doctors per 1,000 patients.[32] In 2005, Italy spent 8.9% of GDP on health care, or US$2,714 per capita. Of that, approximately 76% was government expenditure.[18]
Japan
In Japan, services are provided either through regional/national public hospitals or through private hospitals/clinics, and patients have universal access to any facility, though hospitals tend to charge higher for those without a referral. Public health insurance covers most citizens/residents and pays 70% or more cost for each care and each prescribed drug. Patients are responsible for the remainder (upper limits apply). The monthly insurance premium is 0-50,000 JPY per household (scaled to annual income). Supplementary private health insurance is available only to cover the co-payments or non-covered costs, and usually makes a fixed payment per days in hospital or per surgery performed, rather than per actual expenditure. In 2005, Japan spent 8.2% of GDP on health care, or US$2,908 per capita. Of that, approximately 83% was government expenditure.[18]
Jordan
In comparison to most of its neighbors, Jordan has quite an advanced health care system, although services remain highly concentrated in Amman. Government figures have put total health spending in 2002 at some 7.5 percent of Gross domestic product (GDP), while international health organizations place the figure even higher, at approximately 9.3 percent of GDP. The country’s health care system is divided between public and private institutions. In the public sector, the Ministry of Health operates 1,245 primary health-care centers and 27 hospitals, accounting for 37 percent of all hospital beds in the country; the military’s Royal Medical Services runs 11 hospitals, providing 24 percent of all beds; and the Jordan University Hospital accounts for 3 percent of total beds in the country. The private sector provides 36 percent of all hospital beds, distributed among 56 hospitals. In 1 June 2007, Jordan Hospital (as the biggest private hospital) was the first general specialty hospital who gets the international accreditation (JCI).Treatment cost in Jordan hospitals is less than in other countries. [15]
Kazakhstan
In principle, health care is free. However, bribes often are necessary to obtain needed care. The quality of health care, which remained entirely under state control in 2006, has declined in the post-Soviet era because of insufficient funding and the loss of technical experts through emigration. Between 1989 and 2001, the ratio of doctors per 10,000 inhabitants fell by 15 percent, to 34.6, and the ratio of hospital beds per 10,000 inhabitants fell by 46 percent, to 74. By 2005 those indicators had recovered somewhat, to 55 and 77, respectively. Since 1991, health care has consistently lacked adequate government funding; in 2005 only 2.5 percent of gross domestic product went for that purpose. A government health reform program aims to increase that figure to 4 percent in 2010. A compulsory health insurance system has been in the planning stages for several years. Wages for health workers are extremely low, and equipment is in critically short supply. The main foreign source of medical equipment is Japan. Because of cost, the emphasis of treatment increasingly is on outpatient care instead of the hospital care preferred under the Soviet system. The health system is in crisis in rural areas such as the Aral Sea region, where health is most affected by pollution.[15]
Kuwait
HEALTH SECTOR: Health-care is fairly developed, Kuwaitis (KU) receive medical services at government clinics and hospitals free of charge the Non Kuwaitis (NKU) pay nominal fees. Public health care is maintained by an intricate network of 72 primary health centers spread over the country, these provide general practitioner services, childcare, maternity care, diabetes care, dentistry, preventive medical care, nursing care and pharmaceuticals. Secondary health services are provided by six regional hospitals. These provide surgical and general medical care, specialized clinics and dispensaries. Tertiary health care service centers include: Obstetrics for maternity, Chest, Psychiatric, Neurosurgery, Burns, Orthopedic and Allergy. Kuwait Cancer Control Center (KCCC) provides diagnosis and treatment for cancer patients. Hearing Impairments organs transplant, Physiotherapy and Rehabilitation have special care facilities. Beside government services there are a number of private clinics and hospitals in Kuwait. The Government monitors them, to ensure a high standard of services and regulates the fees charged. Most private hospitals have their own pharmacies. Most private hospitals are also general hospitals with some specialty departments.
Mali
Health in Mali, one of the world’s poorest nations, is greatly affected by poverty, malnutrition, and inadequate hygiene and sanitation. Mali's health and development indicators rank among the worst in the world. In 2000 only 62–65 percent of the population was estimated to have access to safe drinking water and only 69 percent to sanitation services of some kind; only 8 percent was estimated to have access to modern sanitation facilities. Only 20 percent of the nation’s villages and livestock watering holes had modern water facilities.[15]
Mali is dependent on international development organizations and foreign missionary groups for much of its health care. In 2001 general government expenditures on health constituted 6.8 percent of total general government expenditures and 4.3 percent of gross domestic product (GDP), totaling only about US$4 per capita at an average exchange rate. Medical facilities in Mali are very limited, especially outside of Bamako, and medicines are in short supply. There were only 5 physicians per 100,000 inhabitants in the 1990s and 24 hospital beds per 100,000 in 1998. In 1999 only 36 percent of Malians were estimated to have access to health services within a five-kilometer radius.[15]
Malaysia
Health care in Malaysia is divided into private and public sectors. Doctors are required to perform 3 years of service with public hospitals throughout the nation, ensuring adequate coverage of medical needs for the general population. Foreign doctors are encouraged to apply for employment in Malaysia, especially if they are qualified to a higher level.
Malaysian society places importance on the expansion and development of health care, putting 5% of the government social sector development budget into public health care — an increase of more than 47% over the previous figure. This has meant an overall increase of more than RM 2 billion. With a rising and aging population, the Government wishes to improve in many areas including the refurbishment of existing hospitals, building and equipping new hospitals, expansion of the number of polyclinics, and improvements in training and expansion of telehealth. Over the last couple of years they have increased their efforts to overhaul the systems and attract more foreign investment.
There is still a shortage in the medical workforce, especially of highly trained specialists. As a result certain medical care and treatment is available only in large cities. Recent efforts to bring many facilities to other towns have been hampered by lack of expertise to run the available equipment made ready by investments.
The majority of private hospital facilities are in urban areas and, unlike many of the public hospitals, are equipped with the latest diagnostic and imaging facilities.
Mexico
Advances in medicine and increasing health knowledge have increased the life expectancy by 25 years in the second half of the century. While the health of Mexicans has increased in the last four generations, there are millions of citizens who still do not have regular access to health care services. Mexico has adopted a pluralistic health care system. It consists of a combination of public and private health insurance programs. Of the 6.6% of government revenue spent on health, this provides only health insurance to 40% of the population who are privately employed. The health care system has three components: the social security institute, governmental services for the uninsured, and the private sector that is financed almost completely from out of pocket money. Governmental services include all services that are free in rural areas by the Secretariat of Health and family planning, vaccinations, oral rehydration, and emergency services that are free to all parts of the country. The number of public hospitals in Mexico has increased 41% in ten years from 1985 to 1995. Besides public hospitals, private hospitals exist but require pay. The majority of private hospitals are small with 83% of the clinics having less than 14 beds and half of those having less than 5 beds.
Half of Mexican citizens are uninsured and even more pay health costs out of their own pockets. For some families, more than a third of their income goes towards paying for medical needs. Because of the separation between upper and lower class, health inequities also exist when compared to national rates, especially for indigenous communities. For example, 40% of indigenous women have been found to be anemic compared to the national average of 26%. Studies also show that in low income areas, less than 10% of pregnant women deliver their babies in a hospital.
Morocco
According to the United States government, Morocco has inadequate numbers of physicians (0.5 per 1,000 people) and hospital beds (1.0 per 1,000 people) and poor access to water (82 percent of the population) and sanitation (75 percent of the population). The health care system includes 122 hospitals, 2,400 health centers, and 4 university clinics, but they are poorly maintained and lack adequate capacity to meet the demand for medical care. Only 24,000 beds are available for 6 million patients seeking care each year, including 3 million emergency cases. The health budget corresponds to 1.1 percent of gross domestic product and 5.5 percent of the central government budget.[15]
Netherlands
Health care in the Netherlands, has since January 2006 been provided by a system of compulsory insurance backed by a risk equalization program so that the insured are not penalized for their age or health status. This is meant to encourage competition between health care providers and insurers. Children under 18 are insured by the government, and special assistance is available to those with limited incomes. In 2005, the Netherlands spent 9.2% of GDP on health care, or US$3,560 per capita. Of that, approximately 65% was government expenditure.[18]
New Zealand
In New Zealand hospitals are public and treat citizens or permanent residents free of charge and are managed by District Health Boards. Under the Labour coalition governments (1999–2008), there were plans to make primary health care available free of charge. At present government subsidies exist in health care. The cost of visiting a GP ranges from Free to $45.00 for children and from Free to $75.00 for adults under the current subsidies. This system is funded by taxes. The New Zealand government agency PHARMAC subsidizes certain pharmaceuticals depending upon their category. Co-payments exist, however these are lower if the user has a Community Services Card or High User Health Card. In 2005, New Zealand spent 8.9% of GDP on health care, or US$2,403 per capita. Of that, approximately 77% was government expenditure.[18]
Niger
Health care system of Niger suffers from a chronic lack of resources and a small number of health providers relative to population. Some medicines are in short supply or unavailable. There are government hospitals in Niamey (with three main hospitals in Niamey, including the Hôpital National de Niamey and the Hôpital National De Lamordé), Maradi, Tahoua, Zinder and other large cities, with smaller medical clinics in most towns.[33] Medical facilities are limited in both supplies and staff, with a small government health care system supplemented by private, charitable, religious, and Non-government organisation operated clinics and public health programs (such as Galmi Hospital near Birnin Konni and Maradi). Government hospitals, as well as public health programmes, fall under the control of the Nigerien Ministry of Health. A number of private for profit clinics ("Cabinets Médical Privé") operate in Niamey. The total expenditure on health per capita in 2005 was Intl $25. There were 377 Physicians in Niger in 2004, a ratio of 0.03 per 10,000 population. In 2003, 89.2 percent of individual expenditures on health care were "out-of-pocket" (paid by the patient).[34]
Nigeria
Health care provision in Nigeria is a concurrent responsibility of the three tiers of government in the country.[35] However, because Nigeria operates a mixed economy, private providers of health care have a visible role to play in health care delivery. The federal government's role is mostly limited to coordinating the affairs of the university teaching hospitals, while the state government manages the various general hospitals and the local government focus on dispensaries. The total expenditure on health care as % of GDP is 4.6, while the percentage of federal government expenditure on health care is about 1.5%.[36] A long run indicator of the ability of the country to provide food sustenance and avoid malnutrition is the rate of growth of per capita food production; from 1970–1990, the rate for Nigeria was 0.25%.[37] Though small, the positive rate of per capita may be due to Nigeria's importation of food products. Historically, health insurance in Nigeria can be applied to a few instances: free health care provided and financed for all citizens, health care provided by government through a special health insurance scheme for government employees and private firms entering contracts with private health care providers.[38] However, there are few people who fall within the three instances. In May 1999, the government created the National Health Insurance Scheme, the scheme encompasses government employees, the organized private sector and the informal sector. Legislative wise, the scheme also covers children under five, permanently disabled persons and prison inmates. In 2004, the administration of Obasanjo further gave more legislative powers to the scheme with positive amendments to the original 1999 legislative act.[39]
North Korea
North Korea has a national medical service and health insurance system.[15] As of 2000, some 99 percent of the population had access to sanitation, and 100 percent had access to water, but water was not always potable.[15] Medical treatment is free.[15] In the past, there reportedly has been one doctor for every 700 inhabitants and one hospital bed for every 350 inhabitants.[15] Health expenditures in 2001 were 2.5 percent of gross domestic product, and 73 percent of health expenditures were made in the public sector.[15] There were no reported human immuno-deficiency virus/acquired immune deficiency syndrome (HIV/AIDS) cases as of 2007.[15] However, it is estimated that between 500,000 and 3 million people died from famine in the 1990s, and a 1998 United Nations (UN) World Food Program report revealed that 60 percent of children suffered from malnutrition, and 16 percent were acutely malnourished.[15] UN statistics for the period 1999–2001 reveal that North Korea’s daily per capita food supply was one of the lowest in Asia, exceeding only that of Cambodia, Laos, and Tajikistan, and one of the lowest worldwide.[15] Because of continuing economic problems, food shortages and chronic malnutrition prevail in the 2000s.[15]
Norway
Norway has a government run and government financed universal health care system, covering physical and mental health for all and dental health for children under the age of 16. Hospitals are free and doctor visit fees are capped at a fairly low rate. Medicine is market price, but people needing the medicine more than three months a year, gets prescription with high discount. There is also a yearly cap for people with high medical expenses.
Private health care exists: Most adults use private dental care, the public only treat people, for a normal fee, when they have free capacity. Health-related plastic surgery (like burn damage) is covered by the public system, while cosmetic surgery in general is private. There are a number of private psychologists, there are also some private general practice doctors and specialists.
Public health care is financed by a special-purpose income tax on the order of 8-11%, loosely translated as "public benefits fee" (Norwegian: trygdeavgift og Folketrygden). This can be considered a mandatory public insurance, covering not only health care but also loss of income during sick leave, public pension, unemployment benefits, benefits for single parents and a few others. The system is supposed to be self-financing from the taxes.
Norwegian citizens living in Norway are automatically covered, even if they never had taxable income. Norwegian citizens living and working abroad (taxable elsewhere and therefore not paying the "public benefits fee" to Norway) are covered for up to one year after thay move abroad, and must pay an estimated market cost for public health care services. Non-citizens like foreign visitors are covered in full.
According to WHO, total health care expenditure in 2005 was 9% of GDP and paid 84% by government, 15% by private out-of-pocket and ~1% by other private sources[40].
Oman
Oman has one of the best healthcare systems in the world and was ranked at number 8 by the WHO healthcare systems ranking in 2000 [41]. Universal healthcare (including prescriptions and dental care) is provided automatically to all citizens and also to expatriates working in the public sector by the Ministry of Health. Non-eligible individuals such as expatriates working in the private sector and foreign visitors can be treated in the government hospitals and clinics for a very reasonable fee or they can opt for the slightly more expensive private clinics and medical centres. The Ministry of Health also finances the treatment of citizens abroad if the required treatment is not available in Oman. The life expectancy in Oman as of 2007 was 71.6. It had 1.81 doctors per 1000 pop., 1.9 beds per 1000 pop. and an infant mortality rate of 9 per 1000 live births. Health expenditure accounts for 4.5% of government revenue[42].
Pakistan
Pakistan's health indicators, health funding, and health and sanitation infrastructure are generally poor, particularly in rural areas. About 19 percent of the population is malnourished—a higher rate than the 17 percent average for developing countries—and 30 percent of children under age five are malnourished. Leading causes of sickness and death include gastroenteritis, respiratory infections, congenital abnormalities, tuberculosis, malaria, and typhoid fever. The United Nations estimates that in 2003 Pakistan’s human immunodeficiency virus (HIV) prevalence rate was 0.1 percent among those 15–49, with an estimated 4,900 deaths from acquired immune deficiency syndrome (AIDS). AIDS is a major health concern, and both the government and religious community are engaging in efforts to reduce its spread. In 2003 there were 68 physicians for every 100,000 persons in Pakistan. According to 2002 government statistics, there were 12,501 health institutions nationwide, including 4,590 dispensaries, 906 hospitals with a total of 80,665 hospital beds, and 550 rural health centers with a total of 8,840 beds. According to the World Health Organization, Pakistan’s total health expenditures amounted to 3.9 percent of gross domestic product (GDP) in 2001, and per capita health expenditures were US$16. The government provided 24.4 percent of total health expenditures, with the remainder being entirely private, out-of-pocket expenses.
Paraguay
In terms of major indicators, health in Paraguay ranks near the median among South American countries. In 2003 Paraguay had a child mortality rate of 29.5 deaths per 1,000 children, ranking it behind Argentina, Colombia, and Uruguay but ahead of Brazil and Bolivia. The health of Paraguayans living outside urban areas is generally worse than those residing in cities. Many preventable diseases, such as Chagas' disease, run rampant in rural regions. Parasitic and respiratory diseases, which could be controlled with proper medical treatment, drag down Paraguay's overall health. In general, malnutrition, lack of proper health care, and poor sanitation are the root of many health problems in Paraguay.[15]
Health care funding from the national government increased gradually throughout the 1980s and 1990s. Spending on health care rose to 1.7 percent of the gross domestic product (GDP) in 2000, nearly triple the 0.6 percent of GDP spent in 1989. But during the past decade, improvement in health care has slowed. Paraguay spends less per capita (US$13−20 per year) than most other Latin American countries. A 2001 survey indicated that 27 percent of the population still had no access to medical care, public or private. Private health insurance is very limited, with pre-paid plans making up only 11 percent of private expenditures on health care. Thus, most of the money spent on private health care (about 88 percent) is on a fee-for-service basis, effectively preventing the poor population from seeing private doctors. According to recent estimates, Paraguay has about 117 physicians and 20 nurses per 100,000 population.[15]
People's Republic of China
The effective public health work in controlling epidemic disease during the early years of the PRC and, after reform began in 1978, the dramatic improvements in nutrition greatly improved the health and life expectancy of the Chinese people. The 2000 WHO World Health Report - Health systems: improving performance found that China's health care system before 1980 performed far better than countries at a comparable level of development, since 1980 ranks much lower than comparable countries.[43] The end of the famed "barefoot doctor" system was abolished in 1981.
China is undertaking a reform on its health care system. The New Rural Co-operative Medical Care System (NRCMCS) is a new 2005 initiative to overhaul the health care system, particularly intended to make it more affordable for the rural poor. Under the NRCMCS, the annual cost of medical cover is 50 yuan (US$7) per person. Of that, 20 yuan is paid in by the central government, 20 yuan by the provincial government and a contribution of 10 yuan is made by the patient. As of September 2007, around 80% of the whole rural population of China had signed up (about 685 million people). The system is tiered, depending on the location. If patients go to a small hospital or clinic in their local town, the scheme will cover from 70-80% of their bill. If they go to a county one, the percentage of the cost being covered falls to about 60%. And if they need specialist help in a large modern city hospital, they have to bear most of the cost themselves, the scheme would cover about 30% of the bill.[44]
Health care was provided in both rural and urban areas through a three-tiered system. In rural areas the first tier was made up of barefoot doctors working out of village medical centers. They provided preventive and primary-care services, with an average of two doctors per 1,000 people. At the next level were the township health centers, which functioned primarily as out-patient clinics for about 10,000 to 30,000 people each. These centers had about ten to thirty beds each, and the most qualified members of the staff were assistant doctors. The two lower-level tiers made up the "rural collective health system" that provided most of the country's medical care. Only the most seriously ill patients were referred to the third and final tier, the county hospitals, which served 200,000 to 600,000 people each and were staffed by senior doctors who held degrees from 5-year medical schools. Health care in urban areas was provided by paramedical personnel assigned to factories and neighborhood health stations. If more professional care was necessary the patient was sent to a district hospital, and the most serious cases were handled by municipal hospitals. To ensure a higher level of care, a number of state enterprises and government agencies sent their employees directly to district or municipal hospitals, circumventing the paramedical, or barefoot doctor, stage.
Philippines
In 2000 the Philippines had about 95,000 physicians, or about 1 per 800 people. In 2001 there were about 1,700 hospitals, of which about 40 percent were government run and 60 percent private, with a total of about 85,000 beds, or about one bed per 900 people. The leading causes of morbidity as of 2002 were diarrhea, bronchitis, pneumonia, influenza, hypertension, tuberculosis, heart disease, malaria, chicken pox, and measles. Cardiovascular diseases account for more than 25 percent of all deaths. According to official estimates, 1,965 cases of human immunodeficiency virus (HIV) were reported in 2003, of which 636 had developed acquired immune deficiency syndrome (AIDS). Other estimates state that there may have been as many as 9,400 people living with HIV/AIDS in 2001.[15]
Romania
Health care public system has been improved but it is still poor by European standards, and access is limited in rural areas. In 2007 health expenditures were equal to 3.9 percent of gross domestic product. In 2007 there were 2.2 physicians and 6.4 hospital beds per 1,000 people. The system is funded by the National Health Care Insurance Fund, to which employers and employees make mandatory contributions. Private health care system has developed slowly but now consists of 22 private hospitals and more than 240 clinics[45].[15] [46]
Russia
Article 41 of the Constitution of the Russian Federation confirms a citizen's right to state healthcare and medical assistance free of charge.[47] This is achieved through state compulsory medical insurance (OMS) which is free to Russian citizens, funded by obligatory medical insurance payments made by companies and government subsidies.[48][49] Introduction in 1993 reform of new free market providers in addition to the state-run institutions intended to promote both efficiency and patient choice. A purchaser-provider split help facilitate the restructuring of care, as resources would migrate to where there was greatest demand, reduce the excess capacity in the hospital sector and stimulate the development of primary care. Russian Prime Minister Vladimir Putin announced a new large large-scale health care reform in 2011 and pledged to allocate more than 300 billion rubles ($10 billon) in the next few years to improve health care in the country.[50] He also said that obligatory medical insurance tax paid by companies will increase from current 3.1% to 5.1% starting from 2011.[50]
Senegal
The health budget in Senegal has tripled between 1980 and 2000, leading to the Senegalese people leading healthier and longer lives - the life expectancy at birth is approximately 55.34 years for men, 58.09 years for women, and 56.69 years for the entire population. Also, the prevalence rate of AIDS in Senegal is one of the lowest in Africa, at 0.9%. However, large disparities still exist in Senegal's health coverage, with 70% of doctors, and 80% of pharmacists and dentists, living in the nation's capital city, Dakar.
Singapore
Health care in Singapore is mainly under the responsibility of the Singapore Government's Ministry of Health. Singapore generally has an efficient and widespread system of health care. It implements a universal health care system, and co-exists with private health care system. Infant mortality rate: in 2006 the crude birth rate stood at 10.1 per 1000, a very low level attributed to birth control policies, and the crude death rate was also one of the lowest in the world at 4.3 per 1000. In 2006, the total fertility rate was only 1.26 children per woman, the 3rd lowest in the world and well below the 2.10 needed to replace the population. Singapore was ranked 6th in the World Health Organization's ranking of the world's health systems in the year 2000.
Singapore has a universal health care system where government ensures affordability, largely through compulsory savings and price controls, while the private sector provides most care. Overall spending on health care amounts to only 3% of annual GDP. Of that, 66% comes from private sources.[40] Singapore currently has the lowest infant mortality rate in the world (equaled only by Iceland) and among the highest life expectancies from birth, according to the World Health Organization.[51] Singapore has "one of the most successful health care systems in the world, in terms of both efficiency in financing and the results achieved in community health outcomes," according to an analysis by global consulting firm Watson Wyatt.[52] Singapore's system uses a combination of compulsory savings from payroll deductions (funded by both employers and workers) a nationalized catastrophic health insurance plan, and government subsidies, as well as "actively regulating the supply and prices of health care services in the country" to keep costs in check; the specific features have been described as potentially a "very difficult system to replicate in many other countries." Many Singaporeans also have supplemental private health insurance (often provided by employers) for services not covered by the government's programs.[52]
Singapore’s well-established health care system comprises a total of 13 private hospitals, 10 public (government) hospitals and several specialist clinics, each specializing in and catering to different patient needs, at varying costs.
Patients are free to choose the providers within the government or private health care delivery system and can walk in for a consultation at any private clinic or any government polyclinic. For emergency services, patients can go at any time to the 24-hour Accident & Emergency Departments located in the government hospitals.
Singapore's medical facilities are among the finest in the world, with well qualified doctors and dentists, many trained overseas.
Singapore has medical savings account system known as Medisave.
South Africa
In South Africa, parallel private and public systems exist. The public system serves the vast majority of the population, but is chronically underfunded and understaffed. The wealthiest 20% of the population uses the private system and are far better served. This division in substantial ways perpetuates racial inequalities created in the pre-apartheid segregation era and apartheid era of the 20th century. In 2005, South Africa spent 8.7% of GDP on health care, or US$437 per capita. Of that, approximately 42% was government expenditure.[18]
Sudan
Outside urban areas, little health care is available in Sudan, helping account for a relatively low average life expectancy of 57 years and an infant mortality rate of 69 deaths per 1,000 live births, low by standards in Middle Eastern but not African countries. For most of the period since independence in 1956, Sudan has experienced civil war, which has diverted resources to military use that otherwise might have gone into health care and training of professionals, many of whom have migrated in search of more gainful employment. In 1996 the World Health Organization estimated that there were only 9 doctors per 100,000 people, most of them in regions other than the South. Substantial percentages of the population lack access to safe water and sanitary facilities. Malnutrition is widespread outside the central Nile corridor because of population displacement from war and from recurrent droughts; these same factors together with a scarcity of medicines make diseases difficult to control. Child immunization against most major childhood diseases, however, had risen to approximately 60 percent by the late 1990s from very low rates in earlier decades. Spending on health care is quite low—only 1 percent of gross domestic product (GDP) in 1998 (latest data). The United Nations placed the rate of human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS) infection in late 2003 at 2.3 percent for adults, quite low by regional standards. The United Nations suggested, however, that the rate could be as high as 7.2 percent. Between 400,000 and 1.3 million adults and children were living with HIV, and AIDS deaths numbered 23,000. As of late 2004, some 4 million persons in the South had been internally displaced and more than 2 million had died or been killed as a result of two decades of war. Comparable figures for Darfur were 1.6 million displaced and 70,000 dead since fighting began there in early 2003.[15]
Sweden
In Sweden, the publicly funded medical system is comprehensive and compulsory. Physician and hospital services take a small patient fee, but their services are funded through the taxation scheme of the County Councils of Sweden. The board of county councils are appointed by local elections.[53] In 2005, Sweden spent 9.2% of GDP on health care, or US$3,727 per capita. Of that, approximately 82% was public expenditure.[18] Sweden also has a smaller private health care, mostly in bigger cities[54][55], or as centers for preventive health care financed by employers.
Details and patient costs
Prescription medicine costs per year are limited for the patient. When you have paid 1,800 SEK (= 249 USD) to the pharmacy the medicines are paid by the government for the rest of the year. All pharmacies are network connected so you can get your medicines from any pharmacy in the country and the same rules apply as if you only use a single local pharmacy. The prescription is sent through internet to the pharmacy network, so you only have to show your identity card in a pharmacy and the pharmacy computer shows what medicines you should have, when you got each medicine earlier, and what medicines you are allowed to receive at this visit. A year after your prescription was sent to the pharmacy system you call the doctor secretary and ask for the prescription to be renewed for the coming year and you can ask for changes to the prescription. If the doctor or you think you need to visit the doctor or take new tests such a visit is arranged.
There is also a limit on health care fees per year. You pay 150 SEK (= 21 USD) each time you visit a doctor, no matter if he is a private doctor or work at a local health care center or at a big hospital. When you visit a hospital the entrance fee (21 USD) covers all specialist visits the doctor sends you to, like x-ray, rheumatism specialist, heart surgery operation, etc.. The same sum is taken out if you are brought in by an ambulance in an acute situation, but then you get a bill after you have been cured and returned home so you can pay the bill. But after you have paid 800 SEK (= 111 USD) you don't have to pay anything for health care for the rest of the year.
So, to pay for doctor fees and prescribed medicines you never have to pay more than 800 plus 1800 SEK (360 USD) per year.
Plastic surgery is covered by the same rules, if the doctors decide that it is necessary. Unnecessary plastic surgery is paid for in full by the patient. That means that if a woman can convince a doctor that her small, or big, breasts is a serious problem for her she gets a breast enlargement or reduction practically for free. (cost for 2 visits (referring local doctor plus the hospital visit when the operation is made) becomes 42 USD in total). If she can not convince a doctor that she needs bigger or smaller breasts she has to pay around 45,000 SEK = 6,226 USD for the operation.
Dental care is not included in the general health care system, but it is partly subsidized by the government. A lot of swedes want dental care to be fully included in the general health care system, and a growing group of politicians support that.
Switzerland
In Switzerland, compulsory health insurance covers the costs of medical treatment and hospitalization of the insured. The Swiss healthcare system is a combination of public, subsidized private and totally private healthcare providers, where the insured person has full freedom of choice among the providers in his region. Insurance companies independently set their price points for different age groups, but are forbidden from setting prices based on health risk. In 2000, Switzerland topped all European countries’ health care expenditure when calculated as per capita expenditure in US dollar purchasing parity terms.[56]
The Swiss health care system is interesting as it was the last for-profit system in Europe. In the 1990s, after the private carriers began to deny coverage for pre-existing conditions—and when the uninsured population of Switzerland reached 5%--the Swiss held a referendum (1995) and adopted their present system.
Syria
The Baath Party has placed an emphasis on health care, but funding levels have not been able to keep up with demand or maintain quality. Health expenditures reportedly accounted for 2.5 percent of the gross domestic product (GDP) in 2001. Syria’s health system is relatively decentralized and focuses on offering primary health care at three levels: village, district, and provincial. According to the World Health Organization (WHO), in 1990 Syria had 41 general hospitals (33 public, 8 private), 152 specialized hospitals (16 public, 136 private), 391 rural health centers, 151 urban health centers, 79 rural health units, and 49 specialized health centers; hospital beds totaled 13,164 (77 percent public, 23 percent private), or 11 beds per 10,000 inhabitants. The number of state hospital beds reportedly fell between 1995 and 2001, while the population had an 18 percent increase, but the opening of new hospitals in 2002 caused the number of hospital beds to double. WHO reported that in 1989 Syria had a total of 10,114 physicians, 3,362 dentists, and 14,816 nurses and midwives; in 1995 the rate of health professionals per 10,000 inhabitants was 10.9 physicians, 5.6 dentists, and 21.2 nurses and midwives. Despite overall improvements, Syria’s health system exhibits significant regional disparities in the availability of health care, especially between urban and rural areas. The number of private hospitals and doctors increased by 41 percent between 1995 and 2001 as a result of growing demand and growing wealth in a small sector of society. Almost all private health facilities are located in large urban areas such as Damascus, Aleppo, Tartus, and Latakia.[15]
Taiwan (R.O.C.)
The current health care system in Taiwan, known as National Health Insurance (NHI), was instituted in 1995. NHI is a single-payer compulsory social insurance plan which centralizes the disbursement of health care dollars. The system promises equal access to health care for all citizens, and the population coverage had reached 99% by the end of 2004.[57] NHI is mainly financed through premiums, which are based on the payroll tax, and is supplemented with out-of-pocket payments and direct government funding. In the initial stage, fee-for-service predominated for both public and private providers. Most health providers operate in the private sector and form a competitive market on the health delivery side. However, many health care providers took advantage of the system by offering unnecessary services to a larger number of patients and then billing the government. In the face of increasing loss and the need for cost containment , NHI changed the payment system from fee-for-service to a global budget, a kind of prospective payment system, in 2002.
According to T.R. Reid, Taiwan achieves "remarkable efficiency", costing ~6 percent of GDP universal coverage however this underestimates the cost as it is not fully funded and the government is forced to borrow to make up the difference. "And frankly, the solution is fairly obvious: increase the spending a little, to maybe 8 percent of GDP. Of course, if Taiwan did that, it would still be spending less than half of what America spends."[58]
Thailand
Data on health care are out of date, but in 1995 Thailand had 0.3 physicians and 1.9 hospital beds per 1,000 population. In 2002 annual spending on health care amounted to US$321 per person in purchasing power parity (PPP). Total expenditures represented about 4.4 percent of the gross domestic product (GDP); of this amount, 57.1 percent came from public sources and 42.9 percent from private sources. Some 85 percent of the population had access to potable water in 2002, and 99 percent had access to sanitation. Human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS) is a serious problem in Thailand. The United Nations Programme on HIV/AIDS (UNAIDS) reported in November 2004 that the Thai government had launched a well-funded, politically supported, and pragmatic response to the epidemic. As a result, national adult HIV prevalence has decreased to an estimated 1.5 percent of all persons aged 15 to 49 years (or about 1.8 percent of the total population). It was also reported that 58,000 adults and children had died from AIDS since the first case was reported in 1984. The government has begun to improve its support to persons with HIV/AIDS and has provided funds to HIV/AIDS support groups. Public programs have begun to alter unsafe behavior, but discrimination against those infected continues. The government has funded an antiretroviral drug program and, as of September 2006, more than 80,000 HIV/AIDS patients had received such drugs. Highly pathogenic H5N1 avian influenza (bird flu) has been found among birds in Thailand as well as surrounding areas. The government has pledged financial support for the prevention effort, which mainly focuses on changing poultry farming methods. Major infectious diseases in Thailand also include bacterial diarrhea, hepatitis, dengue fever, malaria, Japanese encephalitis, rabies, and leptospirosis.[15]
Thailand introduced universal coverage reforms in 2001, becoming one of only a handful of lower-middle income countries to do so. Means-tested health care for low income households was replaced by a new and more comprehensive insurance scheme, originally known as the 30 baht project, in line with the small co-payment charged for treatment. People joining the scheme receive a gold card which allows them to access services in their health district, and, if necessary, be referred for specialist treatment elsewhere. The bulk of finance comes from public revenues, with funding allocated to Contracting Units for Primary Care annually on a population basis. According to the WHO, 65% of Thailand's health care expenditure in 2004 came from the government, 35% was from private sources.[40] Although the reforms have received a good deal of critical comment, they have proved popular with poorer Thais, especially in rural areas, and survived the change of government after the 2006 military coup. The then Public Health Minister, Mongkol Na Songkhla, abolished the 30 baht co-payment and made the UC scheme free. It is not yet clear whether the scheme will be modified further under the coalition government that came to power in January 2008.[59][60][61]
Trinidad and Tobago
Trinidad and Tobago operates under a two-tier health-care system. That is, there is the existence of both private health-care facilities and public health-care facilities. The Ministry of Health is responsible for leading the health sector. The service provision aspect of public health care has been devolved to newly created entities, the Regional Health Authorities (RHAs). The Ministry of Health is shifting its focus to concentrate on policy development, planning, monitoring and evaluation, regulation, financing and research. Citizens can access free health care at public health care facilities where health insurance is not required. The health-care system in the country is universal as almost all citizens utilise the services provided. Some, though, opt for private health-care facilities for their ailments.
Recently, the government of Trinidad and Tobago has launched CDAP (Chronic Disease Assistance Programme). The Chronic Disease Assistance Programme provides citizens with free prescription drugs and other pharmaceutical items to combat several health conditions.
Turkmenistan
In the post-Soviet era, reduced funding has put the health system in poor condition. In 2002 Turkmenistan had 50 hospital beds per 10,000 population, less than half the number in 1996. Overall policy has targeted specialized impatient facilities to the detriment of basic, outpatient care. Since the late 1990s, many rural facilities have closed, making care available principally in urban areas. President Niyazov’s 2005 proposal to close all hospitals outside Ashgabat intensified this trend. Physicians are poorly trained, modern medical techniques are rarely used, and medications are in short supply. In 2004 Niyazov dismissed 15,000 medical professionals, exacerbating the shortage of personnel. In some cases, professionals have been replaced by military conscripts. Private health care is rare, as the state maintains a near monopoly. Free public health care was abolished in 2004.[15]
United Kingdom
Each of the four countries of the United Kingdom has a separate but co-operating public health care system. For details of healthcare in each country, see: England, Scotland, Northern Ireland, Wales
England
Healthcare in England is mainly provided by England's public health service, the National Health Service, that provides healthcare to all UK permanent residents that is free at the point of need and paid for from general taxation. Though the public system dominates healthcare provision there is no restriction on the operations of private medical providers or insurers. Private health care and a wide variety of alternative and complementary treatments are available for those with health insurance or willing to pay directly themselves. Medical insurers do not usually cover chronic illnesses though there is no restriction on them doing so and only the services of specialists are usually compensatable by the contracts offered.
Northern Ireland
Healthcare in Northern Ireland is mainly provided by the country's public health service, Health and Social Care in Northern Ireland, that provides healthcare to all UK permanent residents that is free at the point of need and paid for from general taxation. Though the public system dominates healthcare provision, private health care and a wide variety of alternative and complementary treatments are available for those with health insurance or willing to pay directly themselves.
Scotland
Healthcare in Scotland is mainly provided by the country's public health service, NHS Scotland, that provides healthcare to all UK permanent residents that is free at the point of need and paid for from general taxation. Though the public system dominates healthcare provision, private health care and a wide variety of alternative and complementary treatments are available for those with health insurance or willing to pay directly themselves.
Wales
Healthcare in Wales is mainly provided by the country's public health service, NHS Wales, that provides healthcare to all UK permanent residents that is free at the point of need and paid for from general taxation. Though the public system dominates healthcare provision, private health care and a wide variety of alternative and complementary treatments are available for those with health insurance or willing to pay directly themselves.
United States
The United States is alone among developed nations in not yet having a universal health care system, although 2010 legislation has laid the ground for one to be fully functioning by 2014.[63][64] Healthcare in the U.S. does, however, have significant publicly funded components. Medicare covers the elderly and disabled with a historical work record, Medicaid is available for some, but not all of the poor,[65] and the State Children's Health Insurance Program covers children of low-income families. The Veterans Health Administration directly provides health care to U.S. military veterans through a nationwide network of government hospitals; while active duty service members, retired service members and their dependents are eligible for benefits through TRICARE. Together, these tax-financed programs cover 27.8% of the population[66] and make the government the largest health insurer in the nation.
Roughly two thirds of urban hospitals in the U.S. are non-profit hospitals and the balance evenly divided between for-profit hospitals and public hospitals.[67][68] The urban public hospitals are often associated with medical schools. For example, the largest public hospital system in the U.S. is the New York City Health and Hospitals Corporation, which is associated with the New York University School of Medicine.
Although public hospitals constitute the greatest percentage of non-federal hospitals, care in the U.S. is generally provided by physicians in private practice and private hospitals. Just over 59% of Americans receive health insurance through an employer, although this number is declining and the employee's expected contribution to these plans varies widely and is increasing as costs escalate . A significant number of people cannot obtain health insurance through their employer or are unable to afford individual coverage. The U.S. Census Bureau estimated that 15.3% of the U.S. population, or 45.7 million people, were uninsured at some time in 2007. More than 38% of the uninsured are in households earning $50,000 or more per year. The census also states that 16.7% of the 39.6 million on Medicaid incorrectly reported they were uninsured.[66] A few states have taken serious steps toward universal health care coverage, most notably Minnesota, Massachusetts and Connecticut, with recent examples being the Massachusetts 2006 Health Reform Statute[69] and Connecticut's SustiNet plan to provide quality, affordable health care to state residents.[70] In 2005, the United States spent 15.2% of GDP on health care, or US$6,347 per capita. Of that, approximately 45% was government expenditure.[18]
The U.S. Congress is currently debating many options for further reforming the U.S. health care system.
United Arab Emirates
Standards of health care are considered to be generally high in the United Arab Emirates, resulting from increased government spending during strong economic years. According to the UAE government, total expenditures on health care from 1996 to 2003 were US$436 million. According to the World Health Organization, in 2004 total expenditures on health care constituted 2.9 percent of gross domestic product (GDP), and the per capita expenditure for health care was US$497. Health care currently is free only for UAE citizens. Effective January 2006, all residents of Abu Dhabi are covered by a new comprehensive health insurance program; costs will be shared between employers and employees. The number of doctors per 100,000 (annual average, 1990–99) is 181. The UAE now has 40 public hospitals, compared with only seven in 1970. The Ministry of Health is undertaking a multimillion-dollar program to expand health facilities⎯hospitals, medical centers, and a trauma center⎯in the seven emirates. A state-of-the-art general hospital has opened in Abu Dhabi with a projected bed capacity of 143, a trauma unit, and the first home health care program in the UAE. To attract wealthy UAE nationals and expatriates who traditionally have traveled abroad for serious medical care, Dubai is developing Dubai Healthcare City, a hospital free zone that will offer international-standard advanced private health care and provide an academic medical training center; completion is scheduled for 2010.[15]
Uzbekistan
In the post-Soviet era, the quality of Uzbekistan’s health care has declined. Between 1992 and 2003, spending on health care and the ratio of hospital beds to population both decreased by nearly 50 percent, and Russian emigration in that decade deprived the health system of many practitioners. In 2004 Uzbekistan had 53 hospital beds per 10,000 population. Basic medical supplies such as disposable needles, anesthetics, and antibiotics are in very short supply. Although all citizens nominally are entitled to free health care, in the post-Soviet era bribery has become a common way to bypass the slow and limited service of the state system. In the early 2000s, policy has focused on improving primary health care facilities and cutting the cost of inpatient facilities. The state budget for 2006 allotted 11.1 percent to health expenditures, compared with 10.9 percent in 2005.[15]
Venezuela
The right to health care is guaranteed in the Venezuelan Constitution. Government campaigns for the prevention, elimination, and control of major health hazards have been generally successful. Immunization campaigns have systematically improved children's health, and regular campaigns to destroy disease-bearing insects and to improve water and sanitary facilities have all boosted Venezuela's health indicators to some of the highest levels in Latin America[71]. The availability of low- or no-cost health care provided by the Venezuelan Institute of Social Security has also made Venezuela's health care infrastructure one of the more advanced in the region. However, despite being the most comprehensive and well funded in the region, the health care system has deteriorated sharply since the 1980s. Government expenditures on health care constituted an estimated 4.1 percent of gross domestic product in 2002. Total health expenditures per capita in 2001 totaled US$386. Per capita government expenditures on health in 2001 totaled US$240.
Vietnam
The overall quality of health in Vietnam is regarded as good, as reflected by 2005 estimates of life expectancy (70.61 years) and infant mortality (25.95 per 1,000 live births). However, malnutrition is still common in the provinces, and the life expectancy and infant mortality rates are stagnating. In 2001 government spending on health care corresponded to just 0.9 percent of gross domestic product (GDP). Government subsidies covered only about 20 percent of health care expenses, with the remaining 80 percent coming out of individuals’ own pockets.[15]
In 1954 the government in the North established a public health system that reached down to the hamlet level. After reunification in 1976, this system was extended to the South. Beginning in the late 1980s, the quality of health care began to decline as a result of budgetary constraints, a shift of responsibility to the provinces, and the introduction of charges. Inadequate funding has led to delays in planned upgrades to water supply and sewage systems. As a result, almost half the population has no access to clean water, a deficiency that promotes such infectious diseases as malaria, dengue fever, typhoid, and cholera. Inadequate funding also has contributed to a shortage of nurses, midwives, and hospital beds. In 2000 Vietnam had only 250,000 hospital beds, or 14.8 beds per 10,000 people, a very low ratio among Asian nations, according to the World Bank.[15]
Yemen
Despite the significant progress Yemen has made to expand and improve its health care system over the past decade, the system remains severely underdeveloped. Total expenditures on health care in 2002 constituted 3.7 percent of gross domestic product. In that same year, the per capita expenditure for health care was very low, as compared with other Middle Eastern countries—US$58 according to United Nations statistics and US$23 according to the World Health Organization. According to the World Bank, the number of doctors in Yemen rose by an average of more than 7 percent between 1995 and 2000, but as of 2004 there were still only three doctors per 10,000 persons. In 2003 Yemen had only 0.6 hospital beds available per 1,000 persons.[15] Health care services are particularly scarce in rural areas; only 25 percent of rural areas are covered by health services, as compared with 80 percent of urban areas. Emergency services, such as ambulance service and blood banks, are non-existent. Most childhood deaths are caused by illnesses for which vaccines exist or that are otherwise preventable. According to the Joint United Nations Programme on HIV/AIDS, in 2003 an estimated 12,000 people in Yemen were living with human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS).[15]
Zimbabwe
Zimbabwe now has one of the lowest life expectancies on Earth - 44 for men and 43 for women,[72] down from 60 in 1990. The rapid drop has been ascribed mainly to the HIV/AIDS pandemic. Infant mortality has risen from 59 per thousand in the late 1990s to 123 per 1000 by 2004.[73] The health system has more or less collapsed: By the end of November 2008, three of Zimbabwe's four major hospitals had shut down, along with the Zimbabwe Medical School and the fourth major hospital had two wards and no operating theatres working.[74] Due to hyperinflation, those hospitals still open are not able to obtain basic drugs and medicines.[75] The ongoing political and economic crisis also contributed to the emigration of the doctors and people with medical knowledge.[76] In August 2008, large areas of Zimbabwe were struck by the ongoing cholera epidemic.
See also
|
|
References
- ↑ Getting there from here New Yorker article. Jan 2009
- ↑ [1]Johns Hopkins University President William Brody (2008) proposed another set of criteria for evaluating the US health systems: Cost, Coverage, Consistency, Complexity and Chronic Illness.
- ↑ Eldis.com. "Social Health Insurance." Retrieved August 18, 2006.
- ↑ "Regional Overview of Social Health Insurance in South-East Asia, World Health Organization. And Overview of Health Care Financing". Retrieved August 18, 2006.
- ↑ Glied, Sherry A. "Health Care Financing, Efficiency, and Equity." National Bureau of Economic Research, March 2008. Accessed March 20th, 2008.
- ↑ How Private Insurance Works: A Primer by Gary Claxton, Institution for Health Care Research and Policy, Georgetown University, on behalf of the Henry J. Kaiser Family Foundation
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 7.9 Elizabeth Docteur and Howard Oxley (2003). Health-Care Systems: Lessons from the Reform Experience. OECD. http://www.oecd.org/dataoecd/5/53/22364122.pdf.
- ↑ European Union Public Health Information System - HIV/Aides page
- ↑ European Union Public Health Information System - Diabetes page
- ↑ European Union Public Health Information System - Smoking Behaviors page
- ↑ "Mirror, Mirror on the Wall: An International Update on the Comparative Performance of American Health Care". The Commonwealth Fund. May 15, 2007. http://www.commonwealthfund.org/Content/Publications/Fund-Reports/2007/May/Mirror--Mirror-on-the-Wall--An-International-Update-on-the-Comparative-Performance-of-American-Healt.aspx. Retrieved March 7, 2009.
- ↑ Organisation for Economic Co-operation and Development. "OECD Health Data 2008: How Does Canada Compare" (pdf). http://www.oecd.org/dataoecd/46/33/38979719.pdf. Retrieved 2009-01-09..
- ↑ Updated statistics from a 2009 report
- ↑ OECD Health Data 2009 - Frequently Requested Data
- ↑ 15.00 15.01 15.02 15.03 15.04 15.05 15.06 15.07 15.08 15.09 15.10 15.11 15.12 15.13 15.14 15.15 15.16 15.17 15.18 15.19 15.20 15.21 15.22 15.23 15.24 15.25 15.26 15.27 15.28 15.29 15.30 15.31 15.32 15.33 15.34 15.35 15.36 15.37 15.38 15.39 15.40 Afghanistan country profile. Library of Congress Federal Research Division (May 2006). This article incorporates text from this source, which is in the public domain.
- ↑ 16.0 16.1 16.2 IDRC Reshaping Health Care in Latin Americahttp://www.idrc.ca/en/ev-35159-201-1-DO_TOPIC.html.
- ↑ 17.0 17.1 Armando Barrientos "Reforming Health Insurance in Argentina and Chile" Health Policy and Planning 15(4): 420
- ↑ 18.00 18.01 18.02 18.03 18.04 18.05 18.06 18.07 18.08 18.09 18.10 18.11 18.12 18.13 18.14 18.15 18.16 "WHO Statistical Information System". World Health Organization. http://www.who.int/whosis/data/Search.jsp. Retrieved 2008-09-23.
- ↑ "Sis Card". http://nl.wikipedia.org/wiki/SIS-kaart. Retrieved 2010-05-01.
- ↑ Worden, Robert L. "Health". A Country Study: Bhutan (Andrea Matles Savada, editor). Library of Congress Federal Research Division (September 1991). This article incorporates text from this source, which is in the public domain.
- ↑ ANS - Agência Nacional de Saúde Suplementar - ANS TABNET
- ↑ United States Department of State, "Cape Verde: Country Specific Information"
- ↑ http://www.cmaj.ca/cgi/reprint/179/12/1289.pdf
- ↑ World Health Organization Assesses the World's Health Systems
- ↑ The Case for Universal Health Care in the United States
- ↑ Health Insurance in Germany - MySME - Resources for Small Business in Germany in the English Language
- ↑ http://www.willamette.edu/centers/publicpolicy/projects/oregonsfuture/PDFvol5no2/countries_healthcare.pdf
- ↑ http://www.who.int/whr/2000/media_centre/press_release/en/
- ↑ Health Care in Italy
- ↑ (Italian) LEA.
- ↑ Health Service/Insurance Industry in Italy
- ↑ Practising physicians per 1000 population, OECD countries, 2005
- ↑ REPUBLIC OF NIGER PRELIMINARY ATLAS OF POVERTY/VULNERABILITY. MAP 8: VILLAGES WITH CLINICS/HOSPITALS. Prepared for The World Bank Technical Department, Africa Region. 6 March 2001.
- ↑ Niger. Country Health System Fact Sheet, 2006. World Health Organisation.
- ↑ Rais Akhtar; Health Care Patterns and Planning in Developing Countries, Greenwood Press, 1991. pp 264
- ↑ Ronald J. Vogel; Financing Health Care in Sub-Saharan Africa Greenwood Press, 1993. pp 18
- ↑ Ronald J. Vogel; Financing Health Care in Sub-Saharan Africa Greenwood Press, 1993. pp 1-18
- ↑ Ronald J. Vogel; Financing Health Care in Sub-Saharan Africa Greenwood Press, 1993. pp 101-102
- ↑ Felicia Monye; 'An Appraisal of the National Health Insurance Scheme of Nigeria', Commonwealth Law Bulletin, 32:3 415-427
- ↑ 40.0 40.1 40.2 World Health Organization Statistical Information System: Core Health Indicators
- ↑ http://www.who.int/whr/2000/en/whr00_en.pdf
- ↑ http://www.moh.gov.om/stat/2008/index_eng.htm
- ↑ WHO World Health report 2000 - Health systems: improving performance
- ↑ The reform of the rural cooperative medical system in the People's Republic of China: interim experience in 14 pilot counties. Authors: Carrin G.1; Ron A.; Hui Y.; Hong W.; Tuohong Z.; Licheng Z.; Shuo Z.; Yide Y.; Jiaying C.; Qicheng J.; Zhaoyang Z.; Jun Y.; Xuesheng L. Source: Social Science and Medicine, Volume 48, Number 7, April 1999, pp.961-972(12) [2]
- ↑ Anuarul statistic 2008.
- ↑ Bribes for basic care in Romania. The Guardian Weekly (March 26th 2008).
- ↑ "The Constitution of the Russian Federation". http://www.constitution.ru/en/10003000-03.htm.
- ↑ "О МЕДИЦИНСКОМ СТРАХОВАНИИ ГРАЖДАН В РОССИЙСКОЙ ФЕДЕРАЦИИ". http://www.krasmed.ru/law/?id=13&m=.
- ↑ "Russia - Unified Social Tax replaced by insurance contributions". http://www.ipmltd.co.uk/index.php/news-events-document-library/latest-news/173-russia-unified-social-tax-replaced-by-insurance-contributions.
- ↑ 50.0 50.1 "Putin says Russia needs major health care reform". http://en.rian.ru/russia/20100420/158669620.html.
- ↑ World Health Organization, "World Health Statistics 2007: Mortality", based on 2005 data.
- ↑ 52.0 52.1 John Tucci, "The Singapore health system – achieving positive health outcomes with low expenditure", Watson Wyatt Healthcare Market Review, October 2004.
- ↑ Dalarna County Council
- ↑ Sophiahemmet,
- ↑ About CityAkuten
- ↑ http://www.euro.who.int/document/e68670.pdf Switzerland: from the series Health Care Systems in Transition, WHO
- ↑ Fanchiang, Cecilia."New IC health insurance card expected to offer many benefits", Taiwan Journal, January 2nd, 2004 Accessed March 28, 2008
- ↑ T.R. Reid "Taiwan Takes Fast Track to Universal Health Care", NPR April 15, 2008.
- ↑ The Universal Coverage Policy of Thailand: An Introduction
- ↑ G20 Health Care: "Health Care Systems and Health Market Reform in the G20 Countries." Prepared for the World Economic Forum by Ernst & Young. January 3, 2006.
- ↑ Hughes D, Leethongdee S (2007). "Universal coverage in the land of smiles: lessons from Thailand's 30 baht health reforms". Health Affairs 26 (4): 999–1008. doi:10.1377/hlthaff.26.4.999. PMID 17630443.
- ↑ OECD Health Data 2009 - Frequently Requested Data. OECD.
- ↑ Insuring America's Health: Principles and Recommendations, Institute of Medicine at the National Academies of Science.
- ↑ The Case For Single Payer, Universal Health Care For The United States.
- ↑ Overview - What is Not Covered, U.S. Department of Health & Human Services
- ↑ 66.0 66.1 "Income, Poverty, and Health Insurance Coverage in the United States:2007" (PDF). U.S. Census Bureau. http://www.census.gov/prod/2008pubs/p60-235.pdf233.pdf. Retrieved 2008-08-26.
- ↑ Public Hospitals, Answers.com
- ↑ GAO Testimony before Committee on Ways and Means, House of Representatives, by David M. Walker, Comptroller General of the United States, May 26, 2005, p.4 (In 2003, of the roughly 3,900 nonfederal, short-term, acute care general hospitals in the United States, the majority—about 62 percent—were nonprofit. The rest included government hospitals (20 percent) and for-profit hospitals (18 percent).)
- ↑ About.com's Pros & Cons of Massachusetts' Mandatory Health Insurance Program
- ↑ http://www.aarp.org/states/ct/advocacy/articles/in_historic_vote_legislature_overrides_sustinet_veto.html
- ↑ "Health and Social Security". http://countrystudies.us/venezuela/20.htm. Retrieved 2010-04-05.
- ↑ "United Nations Statistics Division". http://unstats.un.org/unsd/demographic/products/socind/health.htm. Retrieved 2008-12-07.
- ↑ "No quick fix for Zimbabwe's economy". BBC. 14 April 2008. http://news.bbc.co.uk/2/hi/business/7346042.stm. Retrieved 2008-12-19.
- ↑ "The death throes of Harare's hospitals". BBC. 7 November 2008. http://news.bbc.co.uk/1/hi/world/africa/7714892.stm. Retrieved 2008-12-03.
- ↑ "Zimbabwe: coping with the cholera outbreak". 26 November 2008. http://www.icrc.org/web/eng/siteeng0.nsf/html/zimbabwe-feature-261108?opendocument. Retrieved 2008-12-03.
- ↑ "Zimbabwe cholera deaths near 500". BBC. 2 December 2008. http://news.bbc.co.uk/2/hi/africa/7760088.stm. Retrieved 2008-12-02.
External links
- HRC/Eldis Health Systems Resource Guide provides access to free online research and other resources on health systems in developing countries
- Health Care Systems: An International Comparison, Strategic Policy and Research, Intergovernmental Affairs, May 2001
- Health policies, a list of latest publications by OECD.
|
|||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||